www.elsaad.com
ELSaad Pharma leading, world-class branded healthcare company.
ELSaad Pharmaceuticals is a leading Syrian Pharmaceutical company established in the beginning of 1995 with an aim to serve medical association and Patient with best quality medicines.
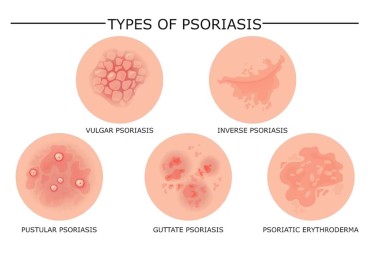
ELSaad Pharmaceuticals is a leader in the Antibiotics and Respiratory segments, and has a strong presence in cardiovascular, Analysis, Urology, Dermatology, General and Local Anesthetic and Anti-Diabetics segments.
ELSaad which has been in the Pharma business for just 18 years has grown through an aggressive strategy of successfully managed acquisitions and alliances. Our portfolio of over 110 products are marketed by a large network of publicity representatives of doctors and pharmacists outnumber the 200 in various Syrian governorates.This is one of the strongest distribution channels in the industry.

www.elsaad.com
New Products